T: 01822 851370 E: [email protected]
October Edition of Casebook from the Rural Health and Care Alliance
 October 2024 Edition
October 2024 Edition
In this month’s edition of the Casebook, we explore ongoing efforts to improve care access in Westmorland and Furness, where community micro-enterprises are expanding support options for older and disabled residents. We also focus on the rural pharmacy crisis, with the RAMP UP campaign pushing for fairer access to NHS medicines in remote areas. Additionally, we examine health inequalities impacting cancer and blood disorder patients in underserved communities, highlighting the need for urgent policy action. Explore these important updates and more!
Creating more choice of care and support in Westmorland and Furness
The area of Westmorland and Furness is a historic and scenic county of northwestern England. Geographically the third largest local authority in England, it is home to approximately 225,000 people. Some of the county towns are in rural areas, which can make it difficult for people to have a choice of local services and supports that work for them.
Community Catalysts partnered with the council to increase the number of community micro-enterprises in the area providing care and support. In 2022, it launched the community micro-enterprise project in the South Lakes, initially in partnership with Cumbria County Council, and with Westmorland and Furness Council after the local government reorganisation in 2023.
Giving people more choice and control over the support they choose
Over 2022-24 the work of the local Catalysts resulted in the creation of a vibrant network of community micro-enterprises that provide a wider choice of care and support to older and disabled people in their homes.
With 125 people receiving 400 hours of support each week, the project has increased the local care and support offer to people. Personal relationships are also at the heart of the community micro-enterprises. While they offer support that is flexible and responsive to the person’s needs, they also foster rich connection with others, which supports people’s quality of life.
Key achievements of the project:
- There is more choice locally for people who draw on care and support and people can choose to have a Direct Payment to pay for their support from a community micro-enterprise.
- Local jobs have been created by community micro-enterprises in South Lakes, Furness and Eden. People can work locally, earn an income and make a positive difference.
- Commissioners, local health and social care teams and people seeking care and support know that good support is available. As a result, people can choose from a range of care and support options locally.
A local social worker said:
“I have found the Community Catalyst and the community enterprises really useful, and I’ve used them a lot… there has 100% been a reduction in unmet need”.
Read the full project report to learn more about the project and what was achieved in Westmorland and Furness.
Small Good Stuff in Cumbria
As part of the community micro-enterprise development project, Community Catalysts offers Small Good Stuff in Cumbria. Small Good Stuff is a directory of care and support services. If people, families or professionals are seeking care and support in the area, they can search the directory to find local community micro-enterprises doing great things.
The impact goes on
The team of Catalysts (group coordinating the project) was key to the success of it, supporting people to set up their own community micro-enterprises. They also supported enterprise leads to set up and run their own peer support networks. This was so community micro-enterprises could continue to benefit from each other.
The team also worked with Westmorland and Furness Council’s commissioning and adult social care teams, who are keen to continue connecting community micro-enterprises with people looking for care and support.
Join the DDA’s RAMP UP Campaign
The Dispensing Doctors’ Association has launched the Rural Access to Medicines and Pharmacy Services Under Pressure (RAMP UP) campaign.
This calls for politicians to use their voice to secure fair pay for NHS GP dispensaries and for rural patients to secure equitable and sustainable access to NHS medicines.
New analysis of pharmacy closures over the last two years shows that rural areas have been hit hardest by a wave of pharmacy closures. Around the country, nearly nine in 10 council areas across England have lost their pharmacies.
BMJ research shows that over a decade 20 per cent of GP practices have closed.
NHS funding for the GP dispensing service – the ‘cost’ element of the dispensing fee – saw a zero uplift this year.
This goes against the aims of the 6 per cent funding award for doctors’ and dentists’ pay accepted by the Government and given to GPs to pay for staff (excluding dispensing staff).
The DDA has published a range of patient briefing materials and template MP letters to support the RAMP UP campaign.
Access these online at:
https://www.dispensingdoctor.org/about-the-dda/dda-political-lobby-documents/

Charity Cancer Campaign Urges Farming Community To ‘Nip It in The Bud’
Farmers and people living in rural communities are being urged to ‘nip it in the bud’ and get checked for early signs of cancer - as part of a new UK-wide campaign by The Farming Community Network (FCN).
FCN is working in partnership with Macmillan Cancer Support to raise awareness of cancer risks, signs and symptoms, and to encourage early detection.
Farmers, farm workers and people living in rural communities can have lower access to cancer services and support due to the nature of their work and rural life, often in isolated areas.
The ‘Nip it in the Bud’ campaign provides a range of useful resources to download or circulate – some focused on specific cancers that farmers can be more at-risk of developing, such as skin cancer, prostate cancer or lung cancer.
Nicky Maynard is a farmer’s wife, originally from Cork in the Emerald Isle, and has lived with her husband and family in Warwickshire for the last 23 years.
In January 2017 she felt a lump in her right breast but initially delayed going to the GP, as she felt fine and there wasn't a female GP available for a few weeks.
After eventually seeing a GP, she quickly received ultrasounds and biopsies and was diagnosed with breast cancer.
Juggling her many roles on the farm whilst undergoing cancer treatment was stressful and she was under a lot of pressure.
Friendships were incredibly important throughout her treatment, and Nicky had friends who really stepped up to the mark after finding out she had cancer. She also received support from Macmillan Cancer Support.
Nicky said: "I am a huge supporter of Macmillan Cancer Support, they ensure that you do not have to go through it alone. I would encourage anyone in a similar position to call them, or ask for information to be sent to you if you are worried.
"I am still not great at listening to my body, but I do force myself to go to the doctor if I am worried about something. Getting to the GP early is essential. Please don’t put it off - Nip it in the Bud."
Nicky has shared her story in the video here:
Alex Phillimore, Head of Communications and Development at The Farming Community Network (FCN), said:
“Some of the signs and symptoms of cancer - such as prolonged pains, tiredness and fatigue - can be missed or overlooked as being ‘part of the job’ in farming. However, we know that the sooner we ‘Nip it in the Bud’ and get checked, the sooner we can find out if something is wrong – and if someone is to receive a cancer diagnosis, the sooner they can undergo treatment. We hope this campaign will encourage people to be more familiar with the early signs of cancer, and to take the necessary steps to get checked and ‘Nip it in the Bud’.”
Launching alongside the Nip it in the Bud campaign is a survey designed to help FCN to better understand current cancer service provisions in rural areas, whilst encouraging people to provide recommendations and suggestions for improvement:
https://www.surveymonkey.com/r/W9DQM5M
Downloadable resources such as graphics, images and information sheets are available on the FCN website:
https://fcn.org.uk/cancersupport/
Examining the impact of health inequalities on cancer and blood disorder patients
The Patients Association is carrying out work to advance health equity by addressing social determinants of health for people living with cancer and blood disorders.
The Patients Association has found that cancer and blood disorder patients that experience health inequalities have worse health and care outcomes and experience of care than those who don’t. Delays in symptom presentation, low uptake of screening programmes and less engagement with mainstream services by at risk communities are underpinned by low health literacy, mistrust of mainstream services, cultural barriers, stigmatisation and poor experiences of care. Variation in care and treatment was found to be associated with experiencing inequalities; these included living in a deprived area, being from a Black and minority ethnic community, experiencing homelessness and having an intellectual disability, among other factors. A lack of training of health professionals, lack of joined-up care, access delays and closures to services were among the factors identified as contributing to poor patient outcomes and experience.
The rising cost-of-living and prohibitively high transportation and medication costs were a particular pain point, further exacerbated by the economic burden of having cancer and/or a blood disorder. There are barriers that underserved communities may face when accessing services and in their experience of care, in the form of lower quality services, delays in testing and diagnosis, lack of participation in shared decision making, and unequal access to digital technology. A consistent thread throughout these experiences was a lack of patient partnership and listening to the patient voice, with patients not being viewed as an expert on their own health condition and not being listened to.
Another barrier to care is transportation costs to attend appointments and treatment. To afford transportation costs, patients/families are cutting back on other items such as recreational and social activities, getting into debt and falling behind on paying bills, selling their possessions or assets, and making difficult decisions between travelling to hospital or paying for essentials.
Patients expressed a deep understanding of the connection between social determinants of health and the impact on health outcomes and wellbeing, with inadequate housing, lack of access to healthy foods, and living in an under-resourced neighbourhood playing a significant role in their lives. This was especially the case for those living in a deprived area where there was less access to adequate healthcare and resources in the community that support health (eg, healthy food shops, gym clubs, social and community groups), resulting in an outsized and negative impact on a patient’s health and wellbeing. Profound impact of living in a deprived area where there was often inadequate health and social care resources available and widespread staffing shortages. For example, since cancer treatment sites are not typically located in deprived areas, residents had to travel across counties, and even to other countries to access treatment. People living in deprived areas seemed to feel resigned to being in poorer health, and not believe that there was assistance available to them.

Government And NHS Must Think Carefully Before Paying The Private Sector To Develop New Facilities
Commenting on recent reports in the national media about private providers bidding the UK government for money to build new facilities for NHS use, Nuffield Trust Senior Policy Analyst Sally Gainsbury said:
“The private sector’s ability to make a significant dent in the NHS waiting list has been limited because it lacks intensive care facilities, meaning private hospitals generally can’t care for patients with serious and complicated illness. Private hospitals are also disproportionately located in the South East, not all across England.
“These reported proposals – submitted to the Treasury by the Independent Healthcare Providers Network – appear to add up to a bid for the government to pay private firms to borrow money from the banks, which they can then invest in building new hospitals, intensive care units, and in recruiting new clinical staff. This begs the question why the government wouldn’t just borrow that money itself, at a far cheaper rate than the private sector can, and add the required capacity to the NHS.
“The NHS needs to think carefully about the benefits of paying the private sector to use its buildings and equipment, and think even harder about the merits of paying the private sector to develop new facilities instead of adding those directly to the NHS. We have seen plenty of instances where these initiatives have cost a great deal of public money for a limited return.”
Pharmacy Closures in Rural Areas: A Growing Healthcare Challenge
A recent report from RSN Member, Healthwatch England has highlighted the growing crisis in community pharmacies across England, which disproportionately affects rural areas.
Between January and December 2023, 436 pharmacies closed permanently, with a further 13,863 instances of temporary closure. This has resulted in the loss of 46,823 hours of pharmacy services—equivalent to more than 5,800 working days. While these closures affect all regions, rural communities, older populations, and areas with fewer GPs per head are being hit hardest.
For rural communities, pharmacies are not just a place to collect prescriptions; they are a lifeline for timely healthcare advice, medications, and support. Yet, the data shows that areas like Norfolk and Waveney, Devon, and Lincolnshire—home to many rural residents—are experiencing some of the highest rates of temporary closures per pharmacy. Norfolk and Waveney alone recorded a staggering 17.48 hours of closure per pharmacy, the highest in England.
Rural Areas and Older Populations at Greater Risk
The data paints a worrying picture for older residents, who rely heavily on these services. Areas with higher percentages of over-60s and over-80s populations, such as Norfolk and Waveney and Lincolnshire, tend to have the most hours of temporary closures. This could mean that those who need access to pharmacies the most are often left without essential services.
The primary reason behind these closures is a shortage of staff, particularly locum pharmacists. Rural areas often struggle to attract and retain healthcare professionals, exacerbating the issue. While Integrated Care Boards (ICBs) have attempted to mitigate the problem, the impact on rural communities continues to worsen.
Healthwatch England is calling for urgent action to address this issue. They recommend that pharmacy teams improve communication around closures and that Integrated Care Boards (ICBs) ensure contingency plans are in place. They stress that more needs to be done to notify patients in advance when pharmacies will be closed, particularly in rural areas where alternative options may be far away.
A national evaluation of pharmacy services, workforce planning, and funding is also being called for, especially given the launch of initiatives like the Pharmacy First service. As pharmacies are increasingly asked to play a bigger role in primary care delivery, it is essential that they are adequately staffed, resourced and accessible.
Mapping the Problem
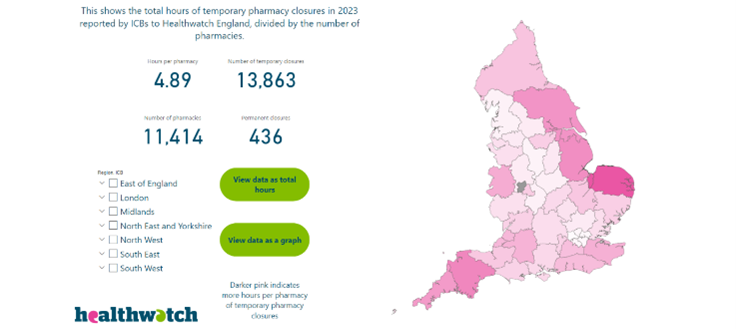 |
To assist in understanding where these closures are having the most impact, Healthwatch has developed a pharmacy closures mapping tool. This tool allows users to explore which areas are most affected, providing valuable data for decision-makers and residents alike. Take a look at the data available for your area HERE. |
For more information on this pressing issue, you can read Healthwatch England’s full briefing HERE and find our more on their website HERE.
Addressing Unmet Needs in Health and Social Care for Older People
Age UK has recently published a crucial report revealing that over 2 million older people in England now have unmet needs for social care. This alarming statistic underscores the pressing issue of inadequate support for many in our aging population, especially in rural areas, where access to necessary services is often limited.
The Age UK report highlights the growing struggle faced by older adults as they navigate a complex health and social care landscape. It emphasises that a significant portion of older individuals is unable to access the essential support needed for daily activities, resulting in diminished quality of life and heightened vulnerability.
The report notes that nearly half of older adults in need of assistance are not receiving adequate help for essential tasks, such as bathing, dressing, and meal preparation. This gap in care often leads to increased isolation, worsening health conditions, and even hospitalisations.
The Rural Context
 |
In rural areas, these challenges are magnified by unique barriers. Limited access to transport, long distances to medical facilities, and an aging demographic create a perfect storm that exacerbates the already critical situation. The Rural Services Network's statistics further illustrate this point: 59% of hard-to-recruit GP specialty training places are in rural regions, highlighting the difficulties in attracting healthcare professionals to serve these communities. |
| Moreover, the report identifies a stark contrast in the proportion of GP-registered patients over 75 years old in rural versus urban settings: 11.5% in rural areas compared to 7.5% in urban regions. This discrepancy not only indicates a higher demand for services in rural areas but also suggests a greater need for tailored health policies that address the specific challenges faced by older adults in these regions. |  |
Implications for Policy and Practice
The findings from Age UK necessitate immediate policy intervention. It is essential to address the root causes of unmet needs in social care, including the underfunding of services, staffing shortages, and the growing demand for support as the population ages.
Key recommendations from the report include:
- Improving Access to Care: Ensure that older adults have easier access to health and social care services, especially in rural areas where transport links are often limited.
- Recruitment and Retention of Healthcare Professionals: Develop targeted recruitment strategies to attract and retain healthcare workers in rural settings, ensuring that these communities are adequately staffed to meet the needs of their aging population.
- Integrating Services: Create integrated health and social care services that facilitate a seamless transition between different types of care, ensuring that older adults receive comprehensive support tailored to their unique needs.
- Public Awareness Campaigns: Raise awareness about the available services for older adults and how to access them, particularly in rural areas where information may not be readily available.
Age UK's report serves as a clarion call for action to address the unmet needs of older adults in England. The Rural Services Network strongly advocates for policy changes that prioritises equitable access to health and social care services, ensuring that every individual can live with dignity and support as they age.
For more detailed insights into the current state of health and social care, refer to Age UK's full report HERE
New Tech Deals Pave the Way for Advances in Cancer Treatment
The Government has announced a series of major investments in cancer research and medical technology, aiming to bolster the country’s life sciences sector and enhance early cancer detection and treatment. The newly unveiled partnerships are expected to advance the development of cutting-edge diagnostic tools and therapies, positioning the UK as a global leader in medical innovation.
New Cancer Therapies and Tech Trials
The latest announcement includes a variety of UK-developed therapies for cancer, which will be tested through a series of new clinical trials. These trials will integrate emerging technologies, including artificial intelligence (AI) tools, to assist NHS professionals in spotting cancers earlier and providing more effective, personalized treatments. This initiative is backed by a combination of public and private sector investments, emphasizing a collaborative effort to deploy innovative diagnostic and treatment approaches.
Establishment of New Health Technology Hubs
One of the key highlights is the creation of five new research hubs across the UK, funded through a £118 million package from UK Research and Innovation. These hubs are designed to support the development of novel health technologies. The new centres will foster collaboration between academic institutions, healthcare providers, and private industry, focusing on various aspects of cancer research and other health challenges.
These hubs will engage in a range of projects, including:
- Imaging Tools for Surgery: Developed by University College London, these tools aim to help surgeons accurately identify and remove cancerous tumors.
- Wearable Technologies: Led by the University of Bristol, these will explore the use of wearable devices to monitor age-related health issues.
- Stem Cell Manufacturing: At the University of Glasgow, this hub will research therapies using adult stem cells, which could help regenerate damaged bone marrow.
Investment in AI and Data for Early Diagnosis
The initiative also includes a £6.4 million investment in a new AI digital pathology data platform, led by NHS England. This platform aims to integrate digital pathology data across the NHS, providing researchers with a secure network to train AI models that can enhance early diagnosis and precision in identifying cancer and other conditions.
Expanding the UK’s Life Sciences Industry
The life sciences industry is already a major contributor to the UK economy, generating £108 billion annually and supporting 300,000 jobs. The Government’s announcement is part of a broader strategy to attract further investment into the sector and stimulate economic growth. The government aims to capitalise on the country’s strong research capabilities and existing industrial base to launch a new wave of high-impact medical products.
Implications for NHS and Health Services
The adoption of these new technologies is seen as a key component in addressing some of the challenges highlighted in the recent Darzi Review, which pointed out that cancer survival rates in England are lower than in many comparable countries. The new initiatives aim to improve patient outcomes by bringing the latest technologies into routine NHS use, ultimately building an NHS that is better equipped to tackle future health challenges.
For more details and a further funding breakdown, read HERE.
We’d love to hear from you - share what you’re proud of
If you have something, you would like us to feature in a future edition, please let us know by clicking here to send us an email.
Spread the word
If you know of other organisations that you think would benefit from joining the Rural Health & Care Alliance, please click here to email us and let us know.
RURAL SERVICES NETWORK
Up to date news on Health and Care
The Rural Services Network provides a useful source of themed news content and data. Check out the latest news on Health & Wellbeing and Vulnerability, where you’ll find articles on a diverse range of rural issues affecting rural communities. You might also find this research on Over 65 Population Projections useful too.
Latest from RSN Member Insights
RSN Member Insights is the place to discover the statistics that define communities within our membership. It is regularly updated with new analyses, and these will be highlighted in the 'What's New' section of the RSN's Weekly Rural Bulletin. The Rural Bulletin also provides a selection of the most rurally topical news items, so do subscribe and encourage your colleagues to subscribe to what is an invaluable weekly periodical.
To make a suggestion of data that would benefit you by being included in the Member Insights section, please email Dan Worth, our Research and Performance Analyst, at [email protected].
| The Rural Health & Care Alliance is a membership organisation administered by the Rural Services Network on behalf of the National Centre for Rural Health & Care. Explore the RHCA service below: |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |









